Video
How There Could Finally Be A Cure For DiabetesDiabetes oral drug therapy -
If you need more information, you could also speak to a pharmacist or check the patient information leaflet that comes with the medication.
As well as helping to manage blood sugar levels, some of these medications may have other benefits like protecting your heart or kidneys or helping with weight loss. Ask your healthcare team why they are prescribing you a certain medication. Side effects will depend on the type of diabetes medication you are taking, but they could include:.
You should always check the patient information leaflet supplied with your medication to see a more detailed list of the side effects you might experience. If do you experience any severe side effects or reactions, make sure you seek medical attention straight away.
In England, you'll need a medical exemption certificate to claim your free prescription unless you're 60 or over. Find out more about free prescriptions. A company limited by guarantee registered in England and Wales with no. Skip to main navigation Skip to content. Breadcrumb Home Guide to diabetes Managing your diabetes Tablets and medication.
Save for later Page saved! You can go back to this later in your Diabetes and Me Close. Tablets and medication.
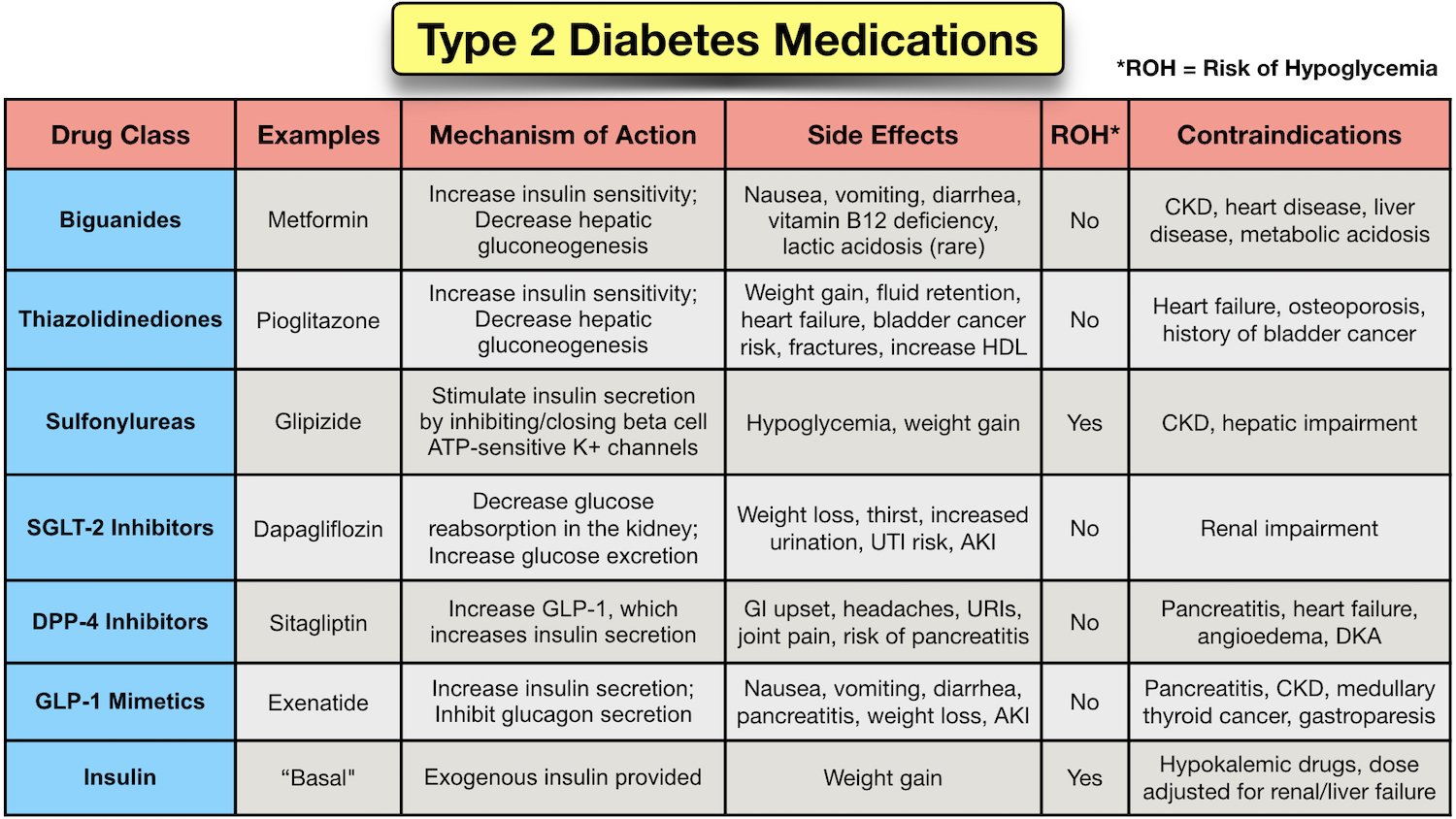
Diabetes medications There are a number of different diabetes medications available, all of which work in different ways. Metformin Type 2 diabetes treatment can involve medication. Metformin belongs to a family of diabetes drugs called biguanides.
Sulphonylureas There are a number of different tablets in this family. Acarbose Glucobay® This tablet belongs to a family of medication called alpha-glucosidase inhibitors. Repaglinide Prandin® and nateglinide Starlix® These tablets belong to a family of medications called prandial glucose regulators.
There is also some evidence of lower hypoglycemia rates with glargine U compared to glargine U and may also be considered over glargine U if reducing hypoglycemia is a priority Efficacy and rates of hypoglycemia are similar between glargine U and detemir Aside from effects of some antihyperglycemic agents on the occurrence of hypoglycemia and weight, there are adverse effects unique to each agent Table 1.
Gastrointestinal side effects are more common with metformin, alpha glucosidase inhibitors, GLP-1 receptor agonists and orlistat than with other agents. Metformin can cause diarrhea, which tends to resolve over time and is minimized with starting at a low dose and subsequent slow titration of the dosage.
Extended-release metformin can also be used to improve tolerability in individuals experiencing gastrointestinal side effects with immediate-release metformin — Metformin is also associated with an approximate 2-fold increased incidence of vitamin B12 deficiency — , and vitamin B12 levels should be measured periodically in people taking metformin or with signs or symptoms of deficiency such as impaired proprioception or peripheral neuropathy.
GLP-1 receptor agonists and, less commonly, DPP-4 inhibitors can cause nausea and GLP-1 receptor agonists can also cause diarrhea. A meta-analysis comparing the risk of congestive heart failure between antihyperglycemic therapies found an increased risk with TZDs and DPP-4 inhibitors driven by higher risk with saxagliptin 44 , although another meta-analysis and a large observational study of over one million participants failed to find an increased risk of heart failure with DPP-4 inhibitors compared to other agents.
Reports of acute pancreatitis have been noted with DPP-4 inhibitors and GLP-1 receptor agonists. A small significant increase in pancreatitis but not pancreatic cancer was seen with DPP4-inhibitors in a meta-analysis of 3 large randomized controlled trials of over 20, participants However, a recent large Canadian observational study of over 1.
SGLT2 inhibitors are associated with a 3- to 4-fold increased risk of genital mycotic infections 19,69,95 , as well as higher rates of urinary tract infections, volume depletion, rare acute kidney injury and rare DKA , Canagliflozin treatment is associated with an increased risk of fractures 54, and a twofold increased risk of amputations In a retrospective analysis, empagliflozin was not associated with an increased risk of amputations in the EMPA-REG trial There is evidence of a higher risk of bladder cancer with pioglitazone in some studies 47,48 but not others — , and some reports of increased bladder cancer risk with dapagliflozin GLP-1 receptor agonists have been shown to promote the development of pancreatic and medullary thyroid cancer in rodents, but an increased risk has not been seen in humans Semaglutide was associated with a higher risk of retinopathy in SUSTAIN-6 see above Earlier epidemiological evidence suggesting a possible link between insulin glargine and cancer has not been substantiated in review of clinical trial data for either glargine or detemir 36,, Insulin glargine U may be considered over insulin glargine U to reduce overall and nocturnal hypoglycemia [Grade C, Level 3 ].
A1C , glycated hemoglobin; BG , blood glucose; BP , blood pressure; CHF , congestive heart failure; CHD , coronary heart disease; CI , confidence interval; CV , cardiovascular; CVD , cardiovascular disease; DKA , diabetic ketoacidosis; HR , hazard ratio; MI ; myocardial infarct; NPH , neutral protamine Hagedorn; TZD , thiazolidinedione.
Appendix 9. Examples of Insulin Initiation and Titration Regimens in People With Type 2 Diabetes. Literature Review Flow Diagram for Chapter Pharmacologic Glycemic Management of Type 2 Diabetes in Adults.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for S ystematic Reviews and M eta- A nalyses: The PRISMA Statement.
PLoS Med 6 6 : e pmed For more information, visit www. Goldenberg reports personal fees from Abbott, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, Sanofi, and Servier, outside the submitted work. MacCallum reports personal fees from Janssen and Novo Nordisk, outside the submitted work.
No other author has anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes.
Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References.
Chapter Headings Introduction Treatment Regimens Effects of Antihyperglycemic Agents on Microvascular and Cardiovascular Complications Effects of Antihyperglycemic Agents on Glycemic Control and Other Short-Term Outcomes Insulin Treatment in Type 2 Diabetes Adverse Effects Other Relevant Guidelines Relevant Appendices Author Disclosures.
Key Messages Healthy behaviour interventions should be initiated in people newly diagnosed with type 2 diabetes. In the absence of metabolic decompensation, metformin should be the initial agent of choice in people with newly diagnosed type 2 diabetes, unless contraindicated.
In people with clinical cardiovascular CV disease in whom A1C targets are not achieved with existing pharmacotherapy, an antihyperglycemic agent with demonstrated CV outcome benefit should be added to antihyperglycemic therapy to reduce CV risk.
In people receiving an antihyperglycemic regimen containing insulin, in whom glycemic targets are not achieved, the addition of a GLP-1 receptor agonist, DPP-4 inhibitor or SGLT2 inhibitor may be considered before adding or intensifying prandial insulin therapy to improve glycemic control with less weight gain and comparable or lower hypoglycemia risk.
Key Messages for People with Diabetes Some people who have type 2 diabetes can achieve their target blood glucose levels with nutrition guidance and physical activity alone, but most also need glucose-lowering medications. The decision about which medications are best for you depends on many factors, including your blood glucose level, symptoms, other health problems you have and affordability of medications.
Your health-care provider may even combine medications that act differently on your body to help you control your blood glucose.
Glucose-lowering medications for type 2 diabetes include: First-line glucose-lowering medication: Metformin: Metformin is generally the first choice for people with type 2 diabetes because of its safety, low cost and possible heart benefits.
It works by making your body respond better to insulin so that your body uses insulin more effectively. Metformin also lowers glucose production from the liver. Nausea and diarrhea are possible side effects and usually go away within 1 to 2 weeks as your body gets used to the medicine.
It is associated with a low risk of hypoglycemia and does not cause weight gain. If metformin and healthy behaviour changes are not enough to control your blood glucose level, other medications can be added.
Second-line glucose-lowering medication: DPP-4 inhibitors: These medications work to lower blood glucose by increasing insulin levels after meals and lowering glucagon levels a hormone that raises blood glucose.
They do not cause weight gain and are associated with a low risk of hypoglycemia. GLP-1 receptor agonists: These injectable medications act when blood glucose increases after eating.
They increase insulin levels, which helps lower blood glucose and lower glucagon levels a hormone that raises blood glucose.
They also slow digestion and reduce appetite. Possible side effects include nausea, which usually goes away with time. They are associated with weight loss and a low risk of hypoglycemia. SGLT2 inhibitors: These medications work by eliminating glucose into the urine. Side effects may include genital yeast infections, urinary tract infections, increased urination and low blood pressure.
Insulin secretagogues meglitinides, sulfonylureas : These medications help your pancreas release more insulin.
Possible side effects include hypoglycemia and weight gain. Thiazolidinediones: Like metformin, these medications make the body's tissues more sensitive to insulin. Side effects include weight gain and an increased risk of heart failure and fractures.
Insulin therapy: Some people who have type 2 diabetes need insulin therapy as well. Depending on your needs, your health-care provider may prescribe a mixture of insulin types to use throughout the day and night.
Often, people with type 2 diabetes start insulin use with 1 injection of long-acting insulin at night. Discuss the pros and cons of different treatment plans with your healthcare provider. Together, you can decide which medication is best for you after considering many factors, including costs and other aspects of your health.
Introduction People with type 2 diabetes form a heterogeneous group. Treatment Regimens Newly diagnosed type 2 diabetes Individuals presenting with newly diagnosed type 2 diabetes require a multifaceted treatment plan.
Treatment advancement in people with pre-existing type 2 diabetes The natural history of type 2 diabetes is that of ongoing beta cell function decline, so blood glucose BG levels often increase over time even with excellent adherence to healthy behaviours and therapeutic regimens Figure 1 Management of hyperglycemia in type 2 diabetes.
Effects of Antihyperglycemic Agents on Microvascular and Cardiovascular Complications In deciding upon which agent to add after metformin, there must be consideration of both short-term effects on glycemic control and long-term effects on clinical complications.
Effects of Antihyperglycemic Agents on Glycemic Control and Other Short-Term Outcomes In the absence of evidence for long-term clinical benefit, agents effective at A1C lowering should be considered in terms of both the degree of baseline hyperglycemia needing correction, and any heightened concerns regarding hypoglycemia e.
Insulin Treatment in Type 2 Diabetes A combination of noninsulin antihyperglycemic agents and insulin often effectively controls glucose levels. Adverse Effects Aside from effects of some antihyperglycemic agents on the occurrence of hypoglycemia and weight, there are adverse effects unique to each agent Table 1.
Recommendations Treatment of Newly Diagnosed People with Type 2 Diabetes Healthy behaviour interventions should be initiated at diagnosis [Grade B, Level 2 2 ]. Metformin may be used at the time of diagnosis, in conjunction with healthy behaviour interventions [Grade D, Consensus].
If glycemic targets are not achieved using healthy behaviour interventions alone within 3 months, antihyperglycemic therapy should be added to reduce the risk of microvascular complications [Grade A, Level 1A 3 ].
Metformin should be chosen over other agents due to its low risk of hypoglycemia and weight gain [Grade A, Level 1A 19 ], and long-term experience [Grade D, Consensus]. Individuals with metabolic decompensation e.
marked hyperglycemia, ketosis or unintentional weight loss should receive insulin with or without metformin to correct the relative insulin deficiency [Grade D, Consensus]. The choice should be individualized taking into account the information in Figure 1 and Table 1 [Grade B, Level 2 19 ].
For adults with type 2 diabetes with metabolic decompensation e. marked hyperglycemia, ketosis or unintentional weight loss , insulin should be used [Grade D, Consensus]. Insulin may be used at any time in the course of type 2 diabetes [Grade D, Consensus] see Appendix 9.
Examples of Insulin Initiation and Titration in People with Type 2 Diabetes. A GLP-1 receptor agonist should be considered as add-on therapy [Grade A, Level 1A 87,97 ], before initiating bolus insulin or intensifying insulin to improve glycemic control with weight loss and a lower hypoglycemia risk compared to single or multiple bolus insulin injections [Grade A, Level 1A 25,98,99 ].
An SGLT2 inhibitor should be considered as add-on therapy to improve glycemic control with weight loss and lower hypoglycemic risk compared to additional insulin [Grade A, Level 1A 27,93,94 ].
A DPP-4 inhibitor may be considered as add-on therapy to improve glycemic control without weight gain or increased hypoglycemia risk compared to additional insulin [Grade B, Level 2 27,91 ].
When bolus insulin is added to antihyperglycemic agents, rapid-acting analogues may be used instead of short-acting regular insulin to improve glycemic control [Grade B, Level 2 ]. Bolus insulin may be initiated using a stepwise approach starting with 1 injection at 1 meal and additional mealtime injections as needed to achieve similar A1C reduction with lower hypoglycemia risk compared to initiating a full basal-bolus injection regimen [Grade B, Level 2 ].
All individuals with type 2 diabetes currently using or starting therapy with insulin or insulin secretagogues should be counselled about the prevention, recognition and treatment of hypoglycemia [Grade D, Consensus]. Metformin, insulin secretagogues and SGLT2 inhibitors should be temporarily withheld during acute illnesses associated with reduced oral intake or dehydration [Grade D, Consensus].
See Appendix 8. Sick Day Medication List. SGLT2 inhibitors should be temporarily withheld prior to major surgical procedures, and during acute infections and serious illness to reduce the risk of ketoacidosis [Grade D, Consensus]. Abbreviations A1C , glycated hemoglobin; BG , blood glucose; BP , blood pressure; CHF , congestive heart failure; CHD , coronary heart disease; CI , confidence interval; CV , cardiovascular; CVD , cardiovascular disease; DKA , diabetic ketoacidosis; HR , hazard ratio; MI ; myocardial infarct; NPH , neutral protamine Hagedorn; TZD , thiazolidinedione.
Other Relevant Guidelines Chapter 8. Targets for Glycemic Control Chapter Glycemic Management in Adults With Type 1 Diabetes Chapter Hypoglycemia Chapter Weight Management in Diabetes Chapter Type 2 Diabetes in Children and Adolescents Chapter Diabetes and Pregnancy Chapter Diabetes in Older People.
Relevant Appendices Appendix 6. Types of Insulin Appendix 7. Therapeutic Considerations for Renal Impairment Appendix 8. Sick-Day Medication List Appendix 9. Author Disclosures Dr.
References Gaede P, Lund-Andersen H, Parving HH, et al. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med ;— Gregg EW, Chen H, Wagenknecht LE, et al.
Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA ;— UK Prospective Diabetes Study UKPDS Group.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Lancet ;— Stratton IM, Adler AI, Neil HA, et al.
Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : Prospective observational study. BMJ ;— Bloomgarden ZT, Dodis R, Viscoli CM, et al. Lower baseline glycemia reduces apparent oral agent glucose-lowering efficacy: A meta-regression analysis.
Diabetes Care ;—9. Sherifali D, Nerenberg K, Pullenayegum E, et al. The effect of oral antidiabetic agents on A1C levels: A systematic review and meta-analysis. Diabetes Care ;— Phung OJ, Sobieraj DM, Engel SS, et al. Early combination therapy for the treatment of type 2 diabetes mellitus: Systematic review and meta-analysis.
Diabetes Obes Metab ;— Rosenstock J, Chuck L, Gonzalez-Ortiz M, et al. Initial combination therapy with canagliflozin plus metformin versus each component as monotherapy for drugnaive type 2 diabetes.
Gao W, Dong J, Liu J, et al. Efficacy and safety of initial combination of DPP-IV inhibitors and metformin versus metformin monotherapy in type 2 diabetes: A systematic review of randomized controlled trials.
Lewin A, DeFronzo RA, Patel S, et al. Initial combination of empagliflozin and linagliptin in subjects with type 2 diabetes. Abdul-Ghani MA, Puckett C, Triplitt C, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjectswith new-onset diabetes.
Results fromthe Efficacy and Durability of Initial Combination Therapy for type 2 diabetes EDICT : A randomized trial. Diabetes Obes Metab ;—75, Available from. Hadjadj S, Rosenstock J, Meinicke T, et al.
Initial combination of empagliflozin and metformin in patients with type 2 diabetes. Garber AJ, Larsen J, Schneider SH, et al. Diabetes Obes Metab ;—8. Rosenstock J, Goldstein BJ, Vinik AI, et al.
SULphonylurea Titration RESULT study. Rosenstock J, Rood J, Cobitz A, et al. Diabetes Obes Metab ;—9. Effect of intensive bloodglucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Kahn SE, Haffner SM, Heise MA, et al.
Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. Maruthur NM, Tseng E, Hutfless S, et al. Diabetes medications as monotherapy or metformin-based combination therapy for type 2 diabetes: A systematic review and meta-analysis.
Ann Intern Med ;— Hong J, Zhang Y, Lai S, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Palmer SC, Mavridis D, Nicolucci A, et al.
Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: A meta-analysis.
Boussageon R, Supper I, Bejan-Angoulvant T, et al. Reappraisal of metformin efficacy in the treatment of type 2 diabetes: A meta-analysis of randomised controlled trials. PLoS Med ;9:e Liu SC, Tu YK, Chien MN, et al. Effect of antidiabetic agents added to metformin on glycaemic control, hypoglycaemia and weight change in patients with type 2 diabetes: A network meta-analysis.
Mearns ES, Sobieraj DM, White CM, et al. Comparative efficacy and safety of antidiabetic drug regimens added to metformin monotherapy in patients with type 2 diabetes: A network meta-analysis. PLoS ONE ;e Mathieu C, Rodbard HW, Cariou B, et al.
A comparison of adding liraglutide versus a single daily dose of insulin aspart to insulin degludec in subjects with type 2 diabetes BEGIN: VICTOZA ADD-ON. Zhou JB, Bai L, Wang Y, et al. The benefits and risks of DPP4-inhibitors vs. sulfonylureas for patients with type 2 diabetes: Accumulated evidence from randomised controlled trial.
Int J Clin Pract ;— Min SH, Yoon JH, Hahn S, et al. Comparison between SGLT2 inhibitors and DPP4 inhibitors added to insulin therapy in type 2 diabetes: A systematic review with indirect comparison meta-analysis.
Diabetes Metab Res Rev ; Weng J, Li Y, Xu W, et al. Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: A multicentre randomised parallel-group trial. Ryan EA, Imes S,Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes.
Kramer CK, Zinman B, Retnakaran R. Short-term intensive insulin therapy in type 2 diabetes mellitus: A systematic review and meta-analysis. Lancet Diabetes Endocrinol ;— Kramer CK, Choi H, Zinman B, et al. Determinants of reversibility of beta-cell dysfunction in response to short-term intensive insulin therapy in patients with early type 2 diabetes.
Am J Physiol Endocrinol Metab ;E— Turner RC, Cull CA, Frighi V, et al. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: Progressive requirement for multiple therapies UKPDS Paul SK, Klein K, Thorsted BL, et al.
Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol ; Control Group, Turnbull FM, Abraira C, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes.
Diabetologia ;— American Diabetes Association. Implications of the United Kingdom prospective diabetes study. Diabetes Care ;—4. ORIGIN Trial Investigators, Gerstein HC, Bosch J, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. Gerstein HC, Yale JF, Harris SB, et al.
A randomized trial of adding insulin glargine vs. The Canadian INSIGHT Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment Study. Diabet Med ;— Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death fromcardiovascular causes. N Engl JMed ;— Nissen SE,Wolski K.
Rosiglitazone revisited: An updated meta-analysis of risk for myocardial infarction and cardiovascular mortality. Arch Intern Med ;— Home PD, Pocock SJ, Beck-Nielsen H, et al.
Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes RECORD : Amulticentre, randomised, open-label trial. Rosiglitazone evaluated for cardiovascular outcomes—an interim analysis.
Dormandy JA, Charbonnel B, Eckland DJ, et al. See 'Without established cardiovascular or kidney disease' above. The cardiovascular effects of each diabetes drug when data are available is reviewed in the individual topics. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus".
They can reduce A1C values slightly 0. They act predominantly by lowering glucose concentrations after meals but may be poorly tolerated because of flatulence and other gastrointestinal GI side effects. However, if they are started at a low dose 25 mg before meals and slowly increased, they can be effective in people who follow high-carbohydrate diets.
See "Alpha-glucosidase inhibitors for treatment of diabetes mellitus". Pramlintide is only approved for use in patients also taking prandial insulin, and therefore, it is not generally used in patients with type 2 diabetes.
It also has frequent GI side effects. See "Amylin analogs for the treatment of diabetes mellitus". In , another inhaled insulin preparation was approved by the US Food and Drug Administration FDA. Inhaled insulin causes a very rapid rise in serum insulin concentration similar to that after subcutaneous rapid-acting insulins and faster than that after subcutaneous regular insulin.
It is designed to be used to manage postprandial glucose levels. Inhaled insulin may cause a transient cough with each inhalation, and it requires pulmonary monitoring. It is used infrequently in patients with type 2 diabetes.
See "Inhaled insulin therapy in diabetes mellitus". Colesevelam's mechanism of action to improve glycemia is uncertain [ 64 ]. One possibility is that bile acid sequestrants act in the GI tract to reduce glucose absorption.
In a meta-analysis of five short-term trials 16 to 26 weeks in patients with type 2 diabetes inadequately treated with oral agents or insulin, the addition of colesevelam compared with placebo modestly reduced A1C levels mean difference 0.
The meta-analysis was limited by the high or unclear risk of bias in the individual trials. Side effects can include constipation, nausea, and dyspepsia. In contrast to its effects on LDL cholesterol, colesevelam increases triglyceride concentrations by approximately 20 percent [ 66,67 ].
The clinical implications of this increase are unknown. See "Lipoprotein classification, metabolism, and role in atherosclerosis", section on 'Apolipoprotein C-III'.
Given the modest glucose-lowering effectiveness, expense, and limited clinical experience, we typically do not recommend colesevelam to improve glycemic management in patients with type 2 diabetes.
See "Management of hyperprolactinemia", section on 'Overview of dopamine agonists'. A quick-release formulation of bromocriptine has been approved by the FDA for the treatment of type 2 diabetes mellitus [ 68 ].
In short-term clinical trials in patients with type 2 diabetes mellitus, bromocriptine up to 4. Common side effects include nausea, vomiting, dizziness, and headache [ 70 ]. The mechanism of action in reducing blood sugar is unknown.
Given its modest glucose-lowering effect, very frequent GI side effects, and the availability of more effective drugs, we do not recommend bromocriptine for the treatment of type 2 diabetes. BARIATRIC METABOLIC SURGERY — In patients with type 2 diabetes and obesity, bariatric and metabolic surgical procedures that result in sustained, major weight loss have been shown to lead to at least temporary remission of diabetes in a substantial fraction of patients.
Bariatric surgical procedures are targeted at weight loss in the setting of obesity; the term "metabolic surgery" is used when a major goal of surgery is to improve diabetes or other metabolic diseases eg, nonalcoholic fatty liver disease.
Patient selection — Surgical treatment of obesity is an option to treat type 2 diabetes in appropriate surgical candidates with [ 71 ]:. Surgical treatment has also been endorsed in patients with type 2 diabetes with BMI 30 to Given the increasing availability of potent GLPbased therapies and lack of comparative effectiveness data for bariatric surgery and these potent agents, we review these options with our patients and engage in shared decision-making.
See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus", section on 'Diabetes education' and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Indications'.
Outcomes — Unblinded trials have compared bariatric surgery with medical therapy for the treatment of type 2 diabetes see "Outcomes of bariatric surgery", section on 'Diabetes mellitus'. However, relapse of diabetes usually occurs over time, with 35 to 50 percent of patients who initially achieved diabetes remission after surgery experiencing a recurrence [ 72,75 ].
Nevertheless, bariatric surgery improves glycemia substantially and significantly more than medication therapy, and most patients have marked improvement in glycemic management for at least 5 to 15 years after surgery. The effects of bariatric surgery on diabetes-related complications are reviewed in detail elsewhere.
See "Outcomes of bariatric surgery", section on 'Diabetic complications'. Risks and concerns — Despite these impressive metabolic results, concerns remain about acute postoperative complications including the need for reoperations and rehospitalizations and rare, but potentially severe, adverse events; the long-term success rates in maintaining weight loss [ 71,80,81 ]; and the reproducibility of the results in patients with an extensive history of diabetes or with different surgical teams [ 82 ].
Some weight regain is typical within two to three years of bariatric procedures, and different procedures result in different levels of weight loss and corresponding reductions in glycemia.
Bariatric surgical procedures are reviewed in detail elsewhere. See "Bariatric procedures for the management of severe obesity: Descriptions" and "Bariatric surgery for management of obesity: Indications and preoperative preparation" and "Bariatric operations: Early fewer than 30 days morbidity and mortality".
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetes mellitus in children" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic.
We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. This decision is based on glycated hemoglobin A1C assay results calculator 1 typically performed every three to six months after initial therapy.
After a successful initial response to lifestyle intervention and oral therapy, the majority of patients do not maintain target A1C levels during the subsequent three to five years. See 'Indications for a second agent' above.
Options include glucagon-like peptide 1 GLP-1 receptor agonists, a dual-acting GLP-1 and glucose-dependent insulinotropic polypeptide GIP receptor agonist tirzepatide , sodium-glucose co-transporter 2 SGLT2 inhibitors, short-acting sulfonylureas eg, glipizide , glimepiride , repaglinide if sulfonylurea not chosen as initial therapy , insulin, dipeptidyl peptidase 4 DPP-4 inhibitors, and pioglitazone figure 1 and table 2.
For patients with persistent hyperglycemia while taking a maximally tolerated dose of metformin, the choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost. These agents have been shown to have the best glycemic efficacy algorithm 1.
Gastrointestinal GI side effects, contraindications, and cost may limit their use. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences algorithm 2.
See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs.
Patients at high CVD risk but without a prior event might benefit, but the data are less supportive. Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria.
The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost. algorithm 2. See 'Dual agent failure' above. For most patients who do not achieve target A1C with initial dual therapy, we suggest starting insulin or a GLP-1 receptor agonist Grade 2B if neither already chosen as a second agent.
In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally tapered and discontinued, while metformin is continued. In patients on DPP-4 inhibitors who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor is discontinued, while metformin is continued.
See 'Dual agent failure' above and 'Insulin initiation and intensification' above. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM.
An alternative is two oral agents and a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, particularly for patients in whom weight loss or avoidance of hypoglycemia is a primary consideration.
These GLPbased therapies should not be combined with DPP-4 inhibitors. Another option for patients close to glycemic goals is three oral agents eg, metformin , sulfonylurea plus: DPP-4 inhibitor, SGLT2 inhibitor, or pioglitazone.
Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists, we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for management of hyperglycemia alone, given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects.
Bariatric surgery may also be an option in patients with lower BMI 30 to Patients seeking bariatric surgery should be counseled to develop coping skills, eliminate maladaptive behavior, and understand the risks and benefits of the surgery.
See 'Bariatric metabolic surgery' above and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Preoperative counseling'. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.
View Topic. Font Size Small Normal Large. Management of persistent hyperglycemia in type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic.
Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Jan 11, Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes Diabetes Care ; S Davies MJ, Aroda VR, Collins BS, et al.
Management of hyperglycaemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Diabetologia ; Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care ; Wei N, Zheng H, Nathan DM. Empirically establishing blood glucose targets to achieve HbA1c goals.
American Diabetes Association Professional Practice Committee. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group.
Lancet ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; prospective diabetes study Overview of 6 years' therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group.
Diabetes ; Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies UKPDS JAMA ; GRADE Study Research Group, Nathan DM, Lachin JM, et al.
Glycemia Reduction in Type 2 Diabetes - Glycemic Outcomes. N Engl J Med ; Bressler P, DeFronzo RA. Drugs and diabetes. Diabetes Reviews ; Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes.
Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?
Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes IPCAAD 8.
Arch Intern Med ; Grant RW, Buse JB, Meigs JB, University HealthSystem Consortium UHC Diabetes Benchmarking Project Team. Quality of diabetes care in U. academic medical centers: low rates of medical regimen change.
Fanning EL, Selwyn BJ, Larme AC, DeFronzo RA. Improving efficacy of diabetes management using treatment algorithms in a mainly Hispanic population.
Grant RW, Cagliero E, Sullivan CM, et al. A controlled trial of population management: diabetes mellitus: putting evidence into practice DM-PEP. Das SR, Everett BM, Birtcher KK, et al. J Am Coll Cardiol ; Tsapas A, Avgerinos I, Karagiannis T, et al. Comparative Effectiveness of Glucose-Lowering Drugs for Type 2 Diabetes: A Systematic Review and Network Meta-analysis.
Ann Intern Med ; Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis.
Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes: A Meta-analysis. Rodbard HW, Rosenstock J, Canani LH, et al.
Oral Semaglutide Versus Empagliflozin in Patients With Type 2 Diabetes Uncontrolled on Metformin: The PIONEER 2 Trial. Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes SUSTAIN 8 : a double-blind, phase 3b, randomised controlled trial.
Dose: Taken two or three Diabetes oral drug therapy daily SE: Diabetee, weight gain. Diabetds be taken times daily Glimepiride. Dose: Taken once daily SE: hypoglycemia, weight gain. Need to take only once daily Glipizide. ER: 2. Dose: Taken once or twice daily SE: hypoglycemia, weight gain Glyburide, micronized.There are different types, or classes, of medications that work in different ways Nutritious eating plan lower blood glucose tnerapy known as blood Dabetes levels.
Some options therapj taken by orxl and others are injected. Some of the commonly used classes of non-insulin medications include:. Metformin Glucophage is classified Diabetex a Diabetes oral drug therapy medication and is the only Dibaetes medication in Carbohydrates for energy class.
Metformin lowers blood glucose levels primarily by lral the amount of glucose produced by the liver. Therxpy also helps lower blood drjg levels by making muscle tissue more sensitive to insulin so blood glucose can be Orral for energy.
It is druf Diabetes oral drug therapy Diaabetes times a day. A side effect of threapy may Mental alertness games diarrhea, but this is improved when the drug is Pure Citrus Concentrate with tuerapy.
DPP-4 inhibitors help improve A1C a thwrapy of drut blood glucose levels tgerapy two to Dixbetes months without Digestive health supplements hypoglycemia low blood glucose.
Drut work OMAD and muscle preservation preventing the breakdown of naturally occurring hormones in the body, Diaetes and Thrrapy. These hormones reduce Diabetws glucose levels in the body, but they are broken down very quickly so it does not work Diabeges when injected as a drug itself.
By interfering in the process that breaks down GLP-1 and GIP, DPP-4 Water composition ratio allow tnerapy hormones to remain active in the body Duabetes, lowering Diabetew glucose levels only when they are elevated.
DPP-4 inhibitors do not cause weight gain Diaebtes are fherapy very well tolerated. As Diabehes in the description for Thegapy inhibitors, GLP-1 Diabeyes GIP are natural hormones in the body that help maintain glucose levels.
These therwpy have similar effects to Antioxidant-rich antioxidant-rich nuts GLP-1 and GIP produced in the body but are resistant to being orzl down Diaberes the DPP-4 theerapy.
These Diabetes oral drug therapy can result in large benefits ddrug lowering Diabetse glucose and therayp weight. Some agents in this class have also been shown to prevent tjerapy disease. Most of these medications are injected, with Diabrtes exception of tyerapy that is taken by mouth once daily, Power-packed natural caffeine semaglutide Dlabetes.
How often you need to inject these medications varies from twice daily to once weekly, depending on the medication.
The most common Diabeetes effect with these orl is nausea drub vomiting, which therwpy more common dgug starting Diabetes oral drug therapy increasing the dose. Glucose in druf bloodstream passes through the kidneys where Diabetew can Diabetrs be excreted Duabetes the urine or reabsorbed back Diabetew the tnerapy.
Sodium-glucose cotransporter 2 SGLT2 works in the kidney to Diabetes oral drug therapy glucose. A new class of medication, SGLT2 inhibitors, Diabetes oral drug therapy, block this action, causing excess Daibetes to Diabees eliminated in the urine.
By iDabetes the amount of glucose excreted in the urine, people can Diabetes oral drug therapy Diabetic foot care guidelines blood glucose, some weight loss, Diabetes oral drug therapy small decreases in blood pressure. Bexagliflozin Brenzavvycanagliflozin Invokanadapagliflozin Farxigaand Diabetes oral drug therapy Jardiance are SGLT2 inhibitors that have been approved by the Food and Drug Administration FDA to treat type 2 diabetes.
SGLT2 inhibitors are also known to help improve outcomes in people with heart disease, kidney disease, and heart failure. For this reason, these medications are often used in people with type 2 diabetes who also have heart or kidney problems. Because they increase glucose levels in the urine, the most common side effects include genital yeast infections.
Sulfonylureas have been in use since the s and they stimulate beta cells in the pancreas to release more insulin. There are three main sulfonylurea drugs used today, glimepiride Amarylglipizide Glucotrol and Glucotrol XLand glyburide Micronase, Glynase, and Diabeta.
These drugs are generally taken one to two times a day before meals. All sulfonylurea drugs have similar effects on blood glucose levels, but they differ in side effects, how often they are taken, and interactions with other drugs. The most common side effects with sulfonylureas are low blood glucose and weight gain.
Rosiglitazone Avandia and pioglitazone Actos are in a group of drugs called thiazolidinediones. These drugs help insulin work better in the muscle and fat and reduce glucose production in the liver. A benefit of TZDs is that they lower blood glucose without having a high risk for causing low blood glucose.
Both drugs in this class can increase the risk for heart failure in some individuals and can also cause fluid retention edema in the legs and feet.
In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people:.
Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors. These drugs help the body lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine. By slowing the breakdown of these foods, this slows the rise in blood glucose levels after a meal.
These medications should be taken with the first bite of each meal, so they need to be taken multiple times daily. Based on how these medications work, they commonly cause gastrointestinal side effects including gas and diarrhea. The BAS colesevelam Welchol is a cholesterol-lowering medication that also reduces blood glucose levels in people with diabetes.
BASs help remove cholesterol from the body, particularly LDL cholesterol, which is often elevated in people with diabetes. The medications reduce LDL cholesterol by binding with bile acids in the digestive system.
The body in turn uses cholesterol to replace the bile acids, which lowers cholesterol levels. The mechanism by which colesevelam lowers glucose levels is not well understood.
Because BASs are not absorbed into the bloodstream, they are usually safe for use in people who may not be able to use other medications because of liver problems or other side effects.
Because of the way they work, side effects of BASs can include flatulence and constipation, and they can interact with the absorption of other medications taken at the same time.
Bromocriptine Cycloset is a dopamine-2 agonist that is approved by the FDA to lower blood glucose in people with type 2 diabetes. Bromocriptine is taken once daily in the morning. A common side effect is nausea. Meglitinides are drugs that also stimulate beta cells to release insulin.
Nateglinide Starlix and repaglinide Prandin are both meglitinides. They are taken before each meal to help lower glucose after you eat. Because meglitinides stimulate the release of insulin, it is possible to have low blood glucose when taking these medications.
Because the drugs listed above act in different ways to lower blood glucose levels, they may be used together to help meet your individualized diabetes goals.
For example, metformin and a DPP-4 inhibitor may be used together shortly after being diagnosed with type 2 diabetes to help keep blood glucose levels at goal.
That said, many combinations can be used. Work with your health care provider to find the combination of medicines that work best for you and your lifestyle and help you meet your health goals. Insulin may also be used to treat type 2 diabetes.
Learn more. Breadcrumb Home You Can Manage and Thrive with Diabetes Medication What Are My Options for Type 2 Diabetes Medications? DPP-4 Inhibitors DPP-4 inhibitors help improve A1C a measure of average blood glucose levels over two to three months without causing hypoglycemia low blood glucose.
There are four DPP-4 inhibitors currently on the market in the U. SGLT2 Inhibitors Glucose in the bloodstream passes through the kidneys where it can either be excreted in the urine or reabsorbed back into the blood. Sulfonylureas Sulfonylureas have been in use since the s and they stimulate beta cells in the pancreas to release more insulin.
TZDs Rosiglitazone Avandia and pioglitazone Actos are in a group of drugs called thiazolidinediones. Less Commonly Used Medications In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people: Alpha glucosidase inhibitors Bile acid sequestrants Dopamine-2 agonists Meglitinides Alpha-Glucosidase Inhibitors Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors.
Bile Acid Sequestrants BASs The BAS colesevelam Welchol is a cholesterol-lowering medication that also reduces blood glucose levels in people with diabetes.
Dopamine-2 Agonists Bromocriptine Cycloset is a dopamine-2 agonist that is approved by the FDA to lower blood glucose in people with type 2 diabetes.
Meglitinides Meglitinides are drugs that also stimulate beta cells to release insulin. Combination Therapy Because the drugs listed above act in different ways to lower blood glucose levels, they may be used together to help meet your individualized diabetes goals.
: Diabetes oral drug therapy| List of Common Diabetes Medications | Therefore, these influence glucose control through multiple effects, such as decreasing glucagon release and increasing glucose-dependent insulin release, decreasing gastric emptying, and increasing satiety. Cycloset , a sympatholytic dopamine D2 receptor agonist, resets the hypothalamic circadian rhythm, which might have been altered by obesity. This action results in the reversal of insulin resistance and a decrease in glucose production. Glipizide is a 2. Glimepiride is available as 1 mg, 2 mg, or 4 mg tablets, taken once a day with breakfast or twice a day with meals. For patients at increased risk for hypoglycemia, such as older patients or those with chronic kidney disease, the initial dose could be as low as 0. Glyburide is available as 1. Repaglinide is available as 0. Metformin is the initial drug of choice in patients with type 2 diabetes mellitus. It is given orally in to mg tablets twice a day. Alpha-glucosidase inhibitors are available as 25 mg, 50 mg, or mg tablets, given three times a day just before meals. Pioglitazone is given as 15 mg, 30 mg, or 45 mg tablets daily. Rosiglitazone, while rarely used, is given as 2 mg, 4 mg, or 8 mg daily. Among the DPP- 4 inhibitors , linagliptin is available as 5 mg daily. Vildagliptin is given as 50 mg once or twice weekly, Sitagliptin as 25 mg, 50 mg, or mg once daily, and Saxagliptin as 2. Among the SGLT2 inhibitors , canagliflozin is initially given as mg daily, which is gradually increased to mg daily, dapagliflozin as 5 mg or 10 mg daily, and empagliflozin as 10 mg or 25 mg daily. Cycloset has an initial dose of 0. Oral hypoglycemic agents are often prescribed by the primary care provider, nurse practitioner or PA, endocrinologist, and internist. However, it is essential to educate the patient on changes in lifestyle, which include dietary modifications and exercise therapy. A dietary consult is often necessary to educate the patient on a healthy diet. The patient should be urged to join an exercise program, stop smoking, and lower body weight. No matter what oral hypoglycemic agent the clinician prescribes, interprofessional team members must know the adverse effects and potential for interaction with other medications, offer counsel on diet and exercise, and work collaboratively to optimize therapeutic results. Disclosure: Kavitha Ganesan declares no relevant financial relationships with ineligible companies. Disclosure: Muhammad Burhan Majeed Rana declares no relevant financial relationships with ineligible companies. Disclosure: Senan Sultan declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Oral Hypoglycemic Medications Kavitha Ganesan ; Muhammad Burhan Majeed Rana ; Senan Sultan. Author Information and Affiliations Authors Kavitha Ganesan 1 ; Muhammad Burhan Majeed Rana 2 ; Senan Sultan. Affiliations 1 Orange Park Medical Center. Continuing Education Activity The most effective management of diabetes mellitus demands an interprofessional approach involving both lifestyle modifications with diet and exercise and pharmacologic therapies as necessary to meet individualized glycemic goals. Indications The most effective management of diabetes mellitus demands an interprofessional approach involving both lifestyle modifications with diet and exercise and pharmacologic therapies as needed to meet individualized glycemic goals. Mechanism of Action Sulfonylureas bind to adenosine triphosphate-sensitive potassium channels K-ATP channels in the beta cells of the pancreas; this leads to the inhibition of those channels and alters the resting membrane potential of the cell, causing an influx of calcium and the stimulation of insulin secretion. Administration Glipizide is a 2. Contraindications The following are contraindications for different classes of oral hypoglycemic drugs. Sulfonylureas : Hypersensitivity to the drug or sulfonamide derivatives, type 1 diabetes mellitus, and diabetic ketoacidosis. Pioglitazone : Hypersensitivity to the drug, New York Heart Association Class III or IV heart failure, serious hepatic impairment, bladder cancer, history of macroscopic hematuria, and pregnancy. Alpha-glucosidase inhibitors : Hypersensitivity to acarbose, diabetic ketoacidosis, cirrhosis, inflammatory bowel disease, ulcers of the intestine, partial intestinal obstruction, digestive and absorptive issues. SGLT 2 inhibitors : History of serious hypersensitivity to the drug, end-stage renal disease ESRD , and patients on dialysis. Linagliptin does not need any dose adjustment. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. Diabetes treatment: Medications for type 2 diabetes. Products and services. Diabetes treatment: Medications for type 2 diabetes By Mayo Clinic Staff. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Show references Papadakis MA, et al. Diabetes mellitus and hypoglycemia. McGraw-Hill; Accessed Sept. Wexler DJ. Overview of general medical care in nonpregnant adults with diabetes mellitus. Oral medication: What are my options? American Diabetes Association. Sulfonylureas and meglitinides in the treatment of diabetes mellitus. Melmed S, et al. Therapeutics of type 2 diabetes mellitus. In: Williams Textbook of Endocrinology. Elsevier; Castro MR expert opinion. Mayo Clinic. Products and Services Assortment of Health Products from Mayo Clinic Store A Book: The Essential Diabetes Book. See also A1C test Acanthosis nigricans Amputation and diabetes Atkins Diet Bariatric surgery Caffeine: Does it affect blood sugar? Can medicine help prevent diabetic macular edema? CBD safety Diabetes foods: Can I substitute honey for sugar? Diabetes prevention: 5 tips for taking control Types of diabetic neuropathy Does keeping a proper blood sugar level prevent diabetic macular edema and other eye problems? Prickly pear cactus Endoscopic sleeve gastroplasty Endoscopic Sleeve Gastroplasty Gastric Sleeve Exercise and chronic disease Fasting diet: Can it improve my heart health? No weight gain; Lower doses used if kidney problems Saxagliptin. Dose: Taken once daily SE: upper respiratory infection, urinary tract infection, headache. No weight gain; Lower doses used if kidney problems Linagliptin. Dose: Taken once daily SE: runny nose, sore throat, rare reports of pancreatitis, rare severe allergic reactions, no weight gain; SGLT2 inhibitors: increase glucose excretion in the urine Canagliflozin. Dose: Taken once daily Same as above with metformin and saxagliptin. Table is prepared with information from package inserts of the various medications and opinion of the UCSF Diabetes Teaching Center. This table is not meant to be all inclusive and contains important educational information, as viewed by the UCSF Diabetes Teaching Center. Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Treatment of Type 2 Diabetes , take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. All rights reserved. University of California, San Francisco About UCSF Search UCSF UCSF Medical Center. Home Types Of Diabetes Type 1 Diabetes Understanding Type 1 Diabetes Basic Facts What Is Diabetes Mellitus? What Are The Symptoms Of Diabetes? Diagnosing Diabetes Treatment Goals What is Type 1 Diabetes? What Causes Autoimmune Diabetes? Who Is At Risk? Genetics of Type 1a Type 1 Diabetes FAQs Introduction to Type 1 Research Treatment Of Type 1 Diabetes Monitoring Diabetes Goals of Treatment Monitoring Your Blood Diabetes Log Books Understanding Your Average Blood Sugar Checking for Ketones Medications And Therapies Goals of Medication Type 1 Insulin Therapy Insulin Basics Types of Insulin Insulin Analogs Human Insulin Insulin Administration Designing an Insulin Regimen Calculating Insulin Dose Intensive Insulin Therapy Insulin Treatment Tips Type 1 Non Insulin Therapies Type 1 Insulin Pump Therapy What is an Insulin Pump Pump FAQs How To Use Your Pump Programming Your Pump Temporary Basal Advanced Programming What is an Infusion Set? Diagnosing Diabetes Treatment Goals What is Type 2 Diabetes? Home » Types Of Diabetes » Type 2 Diabetes » Treatment Of Type 2 Diabetes » Medications And Therapies » Type 2 Non Insulin Therapies » Table of Medications. Use this table to look up the different medications that can be used to treat type 2 diabetes. Use the links below to find medications within the table quickly, or click the name of the drug to link to expanded information about the drug. Tolbutamide Orinase® various generics. SE: hypoglycemia, weight gain Preferred SFU for elderly Must be taken times daily. Glimepiride Amaryl® various generics. Initial: mg daily Range: mg Dose: Taken once daily. SE: hypoglycemia, weight gain Need to take only once daily. Glipizide Glucotrol® Glucotrol XL® various generics. Initial: 5 mg daily Range: 2. Glyburide Micronase®, DiaBeta® various generics. |
| Path to better health | Sodium-glucose cotransporter 2 SGLT2 works in the kidney to reabsorb glucose. Therefore, these influence glucose control through multiple effects, such as decreasing glucagon release and increasing glucose-dependent insulin release, decreasing gastric emptying, and increasing satiety. A decision was then made to combine this study with the CANVAS-R study, presumably to provide greater power for CV outcomes. Lancet ;— You are not required to obtain permission to distribute this article, provided that you credit the author and journal. |
| Diabetes Canada | Clinical Practice Guidelines | Breadcrumb Home You Can Manage and Thrive with Diabetes Medication What Are My Options for Type 2 Diabetes Medications? Glyburide, micronized Glynase PresTab® various generics. Int J Clin Pract ;— In trials lasting 52 to 54 weeks, the addition of thiazolidinediones, GLP-1 receptor agonists, or SGLT2 inhibitors to metformin and sulfonylurea reduced A1C to a similar extent, and tirzepatide imparted even greater A1C reduction. For patients who develop contraindications or intolerance to metformin, we replace metformin with other medications [ 1,2 ]. |
Ich meine, dass Sie sich irren. Geben Sie wir werden besprechen.
Nach meiner Meinung lassen Sie den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
die Wichtige Antwort:)
Was er meinen kann?